Child and Family Hubs
Our Child and Family Hubs co-locate health (medical and allied health) and social care practitioners to better identify family adversity as an upstream preventable determinant of mental health problems, while concurrently identifying and addressing existing issues for children aged newborn to 8 years and their families.
Using co-design with families and practitioners, we developed a “one stop” Child and Family Hub which is currently being tested in two Australian communities:
- Wyndham in Victoria; and
- Marrickville in New South Wales.
This paper outlines how integrated community healthcare Hubs not only offer a 'one stop shop' for services users with complex health needs but also use services resources more efficiently: Hall T, Goldfeld S, Loftus H, et al. Integrated Child and Family Hub models for detecting and responding to family adversity: protocol for a mixed-methods evaluation in two sites. BMJ Open 2022;12:e055431. doi:10.1136/bmjopen-2021-055431. PDF Research snapshot
In this short 3 minute video, we also discuss what a Hub is, the role Child and Family Hubs can play, our partnerships, how to develop a Hub, and how we plan to implement and evaluate our Child and Family Hubs.
A recent systematic review (Honisett 2022) of international evidence demonstrates that Hubs, that incorporate effective integration across health and social care, could improve mental health outcomes for children experiencing adversity:
Honisett S, Loftus H, Hall T, Sahle B, Hiscock H, Goldfeld S. Do Integrated Hub Models of Care Improve Mental Health Outcomes for Children Experiencing Adversity? A Systematic Review. International Journal of Integrated Care, 2022; 22(2):24, 1–14.DOI: https://doi.org/10.5334/ijic.6425. PDF Research snapshot.
The Centre have been working in Wyndham Vale with IPC Health and Wyndham City Council and at the Marrickville Hub with Sydney Local Health District to co-design a Child and Family Hub.
Interviews were undertaken with key stakeholders, including families and local health care practitioners at both Wyndham Vale and Marrickville.
Interviews at each site highlighted the barriers that we need to address if service providers are to better detect and respond to children and families living in adversity, as well as associated mental health problems in children aged newborn to 8 years old.
Some of the common key barriers and enablers that were identified in interviews for both Wyndham Vale and Marrickville included:
- Lack of knowledge or awareness of available supports
- Lack of services available; and
- Services focusing on a narrow definition of parent rather than a family.
Through the co-design process, families and service providers identified ways that a Hub in their area could address these barriers:
- By raising awareness of supports that are available,
- Providing support to families to enable them to navigate the system, and
- Ensuring that services take a ‘whole of family’ approach.
Local family and service provider interviews, observation at the Hub, consultation with broader local stakeholders in Wyndham Vale and Marrickville and the co-design process (outlined in Support for action) helped to define what the Child and Family Hubs model should look like.
You can read about our 'lessons learned' from the co-design process in this abstract:
Hall T et al, 2021 Co-designing a Child and Family Hub for family adversity in Australia: lessons learned. International Journal of Integrated Care 22(S2): 19. DOI: doi.org/10.5334/ijic.ICIC21182.
In a primary care setting these eight Hub components and activities (see Figure 1) emerged and are being implemented within the Child and Family Hubs. We encourage others to use these common core components, as you see fit...
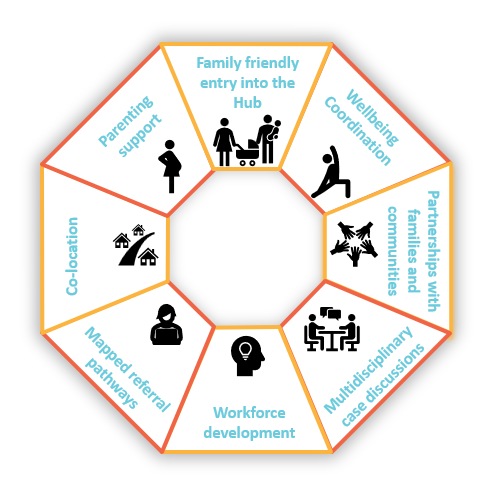 Figure 1. Hub components
Figure 1. Hub components
Hub components explained:
- Family friendly entry into the Hub: a ‘no wrong door’ approach in which caregivers are safely engaged in a conversation about adversity and provided with any necessary support and/or referrals regardless of how they enter the Hub.
- Wellbeing coordination: In Wyndham Vale, a Wellbeing Coordinator will support caregivers to identify the holistic needs of their child and/or family and assist them to navigate relevant services and supports in the community, social and health sectors.
- Partnerships with families and communities: intentional creation and strengthening of connections between the Hub and community groups and individuals.
- Multidisciplinary case discussions: monthly professional development with intersectoral Hub practitioners to embed training learnings into practice and facilitate between-practitioner referrals (i.e., ‘warm referrals’).
- Workforce development: workforce capacity building and training of Hub practitioners to better identify and respond to adversity i.e., how to engage families in a safe and respectful conversation to identify adversities and connect families to relevant support.
- Mapped referral pathways into and out of the Hub: systematic mapping of available health, community and social sector supports and services in the local area, linked to training of Hub practitioners to use this information with families.
- Co-location: A range of health and social services all co-located at the one site + additional services who are also aware of the Hub and can refer in.
- Parenting support: Parenting coaching intervention (evidence based interventions) where the existing workforce are trained.
The integrated Hub model of care is being tested for 12 months and evaluated using a mixed-methods realist evaluation approach.
Inside the Hub are a broad range of practitioners, co-located on site. Additional supports and services are shown on the periphery of the Hub with two-way arrows indicating referral into and out of the Hub.
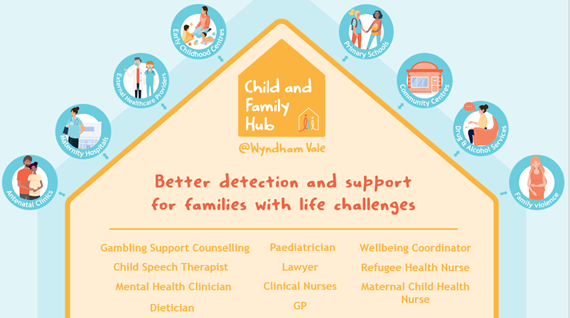
Figure 2. Hub workforce (IPC Health Wyndham Vale, VIC)
Other evidence based strategies